Cold months place steady pressure on the body. Lower temperatures, indoor heating, and reduced sunlight influence how the immune system responds to everyday stressors. When these seasonal factors combine, many people notice more fatigue, more frequent infections, and slower recovery.
Daily habits help maintain a steady immune response during winter. Consistent sleep routines, balanced meals, hydration, and basic self-care support the body’s natural defenses.
Why Cold Weather Challenges the Immune System

Cold temperatures influence several systems that protect the body from illness. Cold exposure reduces several immune defenses. Research shows that severe chilling suppresses important immune functions, including natural-killer cells.
This weakened response makes it easier for viruses to enter the body during cold weather. Indoor heating also lowers humidity, which dries the protective lining of the respiratory tract.
Research shows that winter conditions support faster viral spread. People spend more time indoors with limited ventilation. Surfaces collect germs, and shared environments increase the chance of exposure. Shortened daylight hours influence the internal clock, which affects hormones related to sleep and immune activity.
Common winter pressures include:
- Cold air that reduces local immune defense
- Indoor heating that dries the respiratory tract
- Limited fresh air circulation
- More time in shared indoor spaces
- Less sunlight, which affects energy and sleep patterns
These factors create a setting where immune defenses work harder each day, increasing the likelihood of infections during cold seasons.
For example, indoor heating lowers relative humidity, which dries the respiratory tract. When the air becomes too dry, the mucus layer thickens and mucociliary clearance slows.
This weakens the physical barrier in the nose and throat and makes it easier for viruses and bacteria to enter and infect the body.
How Seasonal Changes Affect People With Chronic Conditions

Seasonal shifts often place extra pressure on people who manage chronic conditions. Cold air can tighten airways for individuals with asthma. Joint stiffness increases for many people with arthritis. Heart and metabolic conditions may also become harder to stabilize because the body uses more energy to stay warm.
Winter conditions may produce the following effects:
- Higher inflammation in people with joint and muscle disorders
- Greater airway sensitivity in asthma and COPD
- More fatigue for those managing endocrine or autoimmune conditions
- Slower recovery from mild infections
- Fluctuations in blood pressure and blood sugar
Crowded indoor settings increase exposure to viruses. For those with chronic conditions, even mild respiratory infections can extend recovery time and increase symptom instability.
Stress from shorter days, holidays, and disrupted routines adds further pressure to the immune system. Understanding these seasonal influences helps people adjust habits before symptoms intensify.
Understanding Baseline Immunity and Daily Protection
Baseline immunity refers to the steady level of immune function the body maintains on a daily basis. This baseline depends on consistent habits that support normal physiological processes. When baseline immunity stays stable, the body manages seasonal challenges with fewer fluctuations.
Daily protection includes simple actions that support this baseline. These actions strengthen routine functions such as tissue repair, circulation, and cellular defense.
People do not need complex strategies to support baseline immunity. Regular patterns often provide more stability than occasional large changes.
Helpful daily protection habits include:
- Consistent sleep schedules
- Balanced meals with varied nutrients
- Hydration throughout the day
- Light daily movement
- Limited smoking and reduced alcohol intake
- Regular handwashing
- Monitoring symptoms for early changes
A stable baseline acts as a foundation for winter health. It helps the immune system respond steadily when environmental pressures rise.
The Role of Consistent Sleep in Keeping the Body Steady

Sleep supports immune function by allowing the body to repair tissues and regulate inflammation. During sleep, the body releases proteins that help fight infection. When sleep becomes irregular, these processes slow down. People with chronic conditions may notice more frequent flare-ups or slower recovery when sleep patterns change.
Cold months introduce several challenges to sleep quality. Shorter days affect the internal clock, while indoor heating can cause dryness that interrupts rest. Stress and irregular schedules during the winter holidays also disrupt sleep routines.
Consistent sleep supports winter health through:
- Better immune regulation
- Improved energy levels
- More stable hormone patterns
- Reduced inflammation
- Better recovery from mild infections
Helpful sleep habits include keeping regular sleep times, reducing late-night screen use, choosing calmer evening activities, and maintaining a comfortable bedroom temperature. These small adjustments help the body maintain steady immune function through cold seasons.
Discover more about why rest and balanced activity support immune health in our post: Sleep, Movement, and Immunity: Why Rest Matters More Than You Think
Food Patterns That Support Day-to-Day Immune Strength
Daily food choices influence immune function throughout the year. During cold months, many people shift toward heavier meals, but balanced nutrition remains important for steady immune performance.
Nutrients such as vitamins A, C, D, and E support immune cell activity. Protein helps maintain muscle strength and tissue repair, which contribute to overall health.
Helpful winter food patterns include:
- Fruits such as apples, berries, and oranges
- Vegetables such as carrots, greens, and peppers
- Lean protein from poultry, fish, eggs, and beans
- Whole grains such as oats, brown rice, and whole wheat
- Nuts, seeds, and legumes for healthy fats
- Limited processed snacks high in sugar or salt
Warm soups with vegetables and protein offer comfort and balanced nutrition without overwhelming the digestive system. Consistent, moderate eating patterns help maintain stable energy and steady immune performance.
Discover more about the nutrients that support steady immune function in our post: Foods That Naturally Support Your Immune System
Hydration During Colder Months and Why It Often Drops

Hydration often decreases during cold months because lower temperatures reduce thirst signals. People may feel less inclined to drink water even though the body continues to lose fluid through breathing, indoor heating, and daily activity.
Dry indoor air increases water loss from the skin and respiratory tract, which creates a greater need for hydration.
Low hydration affects immune performance by reducing circulation and drying protective tissues. Dry nasal passages trap fewer germs, and thicker mucus makes it harder for the respiratory system to clear irritants.
People with chronic conditions may notice increased symptoms when hydration drops.
Helpful hydration habits include:
- Drinking water consistently throughout the day
- Adding warm herbal drinks for comfort
- Eating water-rich foods such as soups, fruits, and vegetables
- Keeping a water bottle accessible during home or work activities
Stable hydration supports daily immune strength and helps the body manage winter conditions with less strain.
Physical Activity That Supports Stability Without Overexertion
Physical activity supports circulation, muscle function, and immune health, but winter conditions may make daily movement harder. People with chronic conditions often benefit from routines that keep the body active without creating strain.
Gentle, steady activity helps maintain joint comfort, respiratory strength, and overall energy levels. The goal is consistency rather than intensity.
Helpful forms of winter movement include:
- Light walking indoors or outdoors on safe surfaces
- Stretching routines that support flexibility
- Low-impact exercises such as stationary cycling or swimming
- Chair-based exercises for individuals with mobility limits
- Short movement breaks during long periods of sitting
Winter weather may limit outdoor time, so indoor options become more important. People can follow simple video routines, create small circuits at home, or break activity into shorter sessions to prevent fatigue.
Monitoring symptoms before and after exercise helps avoid overexertion. When movement stays moderate and steady, the body maintains circulation, which supports comfort and daily stability throughout colder months.
Managing Stress to Prevent Flare-Ups and Fatigue

Stress affects immune activity and may influence chronic conditions. During winter, shorter daylight hours, holiday schedules, and disrupted routines can increase stress. Stress hormones place additional pressure on the immune system and may contribute to flare-ups, fatigue, and slower recovery.
Helpful stress-management practices include:
- Deep breathing exercises
- Short mindfulness sessions
- Light stretching throughout the day
- Journaling to organize thoughts
- Calming hobbies such as reading or music
- Limiting continuous news or screen exposure
Social support also helps reduce stress. Staying connected through phone calls, messages, or small gatherings provides emotional balance during colder months. Simple outdoor walks can also improve stress levels when the weather allows.
Predictable routines support emotional stability. Regular sleep patterns, set meal times, and time management help reduce mental strain.
People with chronic conditions benefit from checking in with healthcare professionals when stress increases symptoms. Steady stress control supports immune performance and daily comfort during winter.
Learn more about how stress influences the immune system and what helps in our post: How Stress Affects Immunity and Simple Ways to Protect It
Indoor Air Quality and Reducing Irritants at Home
Indoor air quality often declines during cold months because people spend more time inside with limited ventilation. Heating systems dry the air, and irritants such as dust, pet dander, and cleaning residues accumulate more easily.
Poor air quality affects respiratory health and may aggravate chronic conditions, including asthma, allergies, and sinus issues.
Simple ways to support indoor air quality include:
- Opening windows for short periods to circulate fresh air
- Using a humidifier to maintain moderate moisture levels
- Dusting and vacuuming regularly
- Washing bedding and pet items consistently
- Reducing strong fragrances from candles or sprays
- Keeping heating filters clean
Plants may support air freshness by adding moisture, though they should be maintained properly to avoid mold buildup. People with respiratory conditions benefit from monitoring humidity levels and avoiding smoke exposure indoors.
Cleaner air reduces irritation in the throat and airways, which helps the immune system maintain steady function throughout winter.
When and How Supplements Can Be Supportive
Supplements may support immune health during cold months, but they should be considered with guidance from healthcare professionals.
Supplements do not replace balanced meals, sleep, hydration, or medication routines. Instead, they may support areas where nutrients become harder to maintain due to seasonal changes.
Common supplements used in winter include:
- Vitamin D, due to reduced sunlight
- Vitamin C for immune support
- Zinc to support healing and cellular activity
- Omega-3 fatty acids for general wellness
People should avoid taking supplements without proper discussion, especially if they have chronic conditions.
Some supplements may interact with medications or may not be recommended for certain health concerns. A healthcare provider can identify safe options, proper timing, and appropriate dosages.
Consistent habits remain the foundation of immune support, with supplements used only when needed. When chosen with guidance, supplements may support steadier health during colder months.
Medication Routines and Staying Consistent Through Seasonal Changes
Medication routines support stability for many chronic conditions. Cold weather may influence symptoms, which makes consistency even more important. Missed doses or irregular schedules can increase flare-ups, reduce symptom control, and place additional pressure on the immune system.
Helpful practices for maintaining medication routines include:
- Setting reminders on phones or clocks
- Using pill organizers
- Keeping medications in a visible location that stays cool and dry
- Reviewing refills early to avoid shortages
- Scheduling regular check-ins with healthcare providers
Winter disruptions such as holidays, travel, or altered routines may interfere with medication schedules. Planning reduces these interruptions. People should also review dosing instructions to confirm storage needs, timing, and any changes recommended for the season.
When medication routines stay consistent, the immune system works under steadier conditions. This helps reduce symptom swings and supports overall health during winter.
Early Warning Signs That the Body Needs Rest or Adjustment
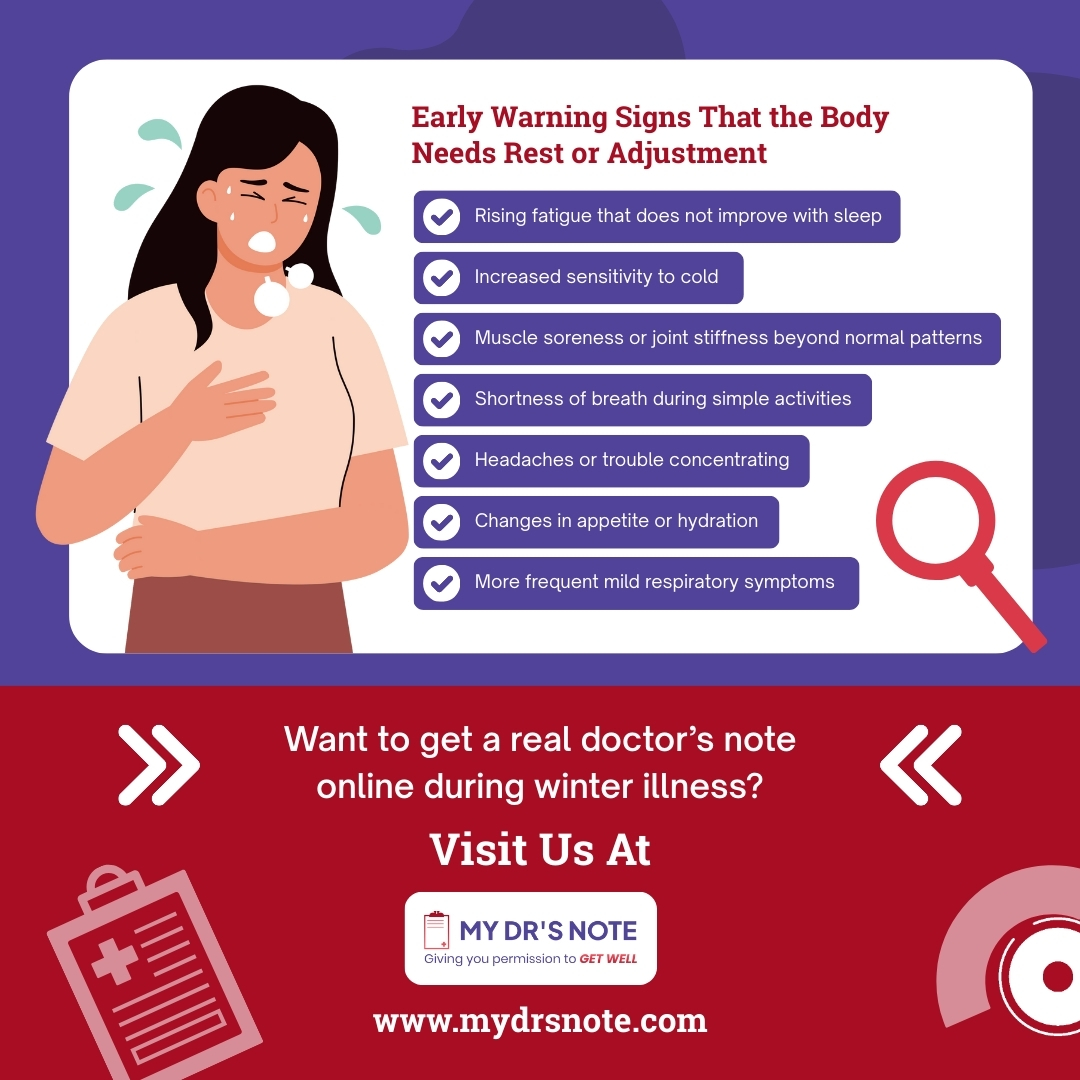
The body often sends clear signals when it becomes strained during cold months. Recognizing these early signs helps prevent symptom flare-ups and reduces the pressure on the immune system.
People with chronic conditions benefit from watching for small changes, as early adjustments may prevent more difficult days ahead.
Common early warning signs include:
- Rising fatigue that does not improve with sleep
- Increased sensitivity to cold
- Muscle soreness or joint stiffness beyond normal patterns
- Shortness of breath during simple activities
- Headaches or trouble concentrating
- Changes in appetite or hydration
- More frequent mild respiratory symptoms
These signs indicate that the body is working harder than usual. When these symptoms appear, adjustments may help, such as resting more, improving hydration, or spacing out daily tasks.
Monitoring patterns over several days helps identify whether symptoms are temporary or developing into more serious concerns. Early action supports immune stability and helps maintain daily comfort through the season.
How Weather Changes Influence Inflammation and Pain Levels
Cold weather often leads to higher discomfort for people who experience chronic inflammation or pain. Temperature drops may cause blood vessels to tighten, which limits circulation to joints and muscles.
This reduced flow can increase stiffness and heighten pain sensations. Sudden weather changes, such as shifts in air pressure, may also intensify symptoms for some individuals.
Common triggers during cold weather include:
- Lower temperatures that tighten muscles
- Decreased circulation
- Reduced outdoor movement
- Higher indoor inactivity
- Shifts in barometric pressure
These conditions make daily tasks feel harder and may contribute to more fatigue. Warm clothing, light stretching, and gentle activity help maintain movement and comfort.
Hydration also supports tissue health, which may reduce stiffness. Recognizing how the weather affects inflammation allows individuals to adjust their routines early and reduce discomfort throughout the day.
How to Prepare for Outdoor Exposure in Low Temperatures
Cold temperatures place additional stress on the body, especially for individuals with chronic conditions.
Preparing before going outdoors helps protect circulation, breathing, and joint comfort. Even brief exposure to low temperatures can affect the respiratory and cardiovascular systems, so planning ahead supports safer winter activity.
Helpful steps before outdoor exposure include:
- Wearing layered clothing that traps warmth
- Using scarves, gloves, and hats to reduce heat loss
- Choosing socks and shoes that keep feet dry
- Allowing a few minutes indoors to warm up before leaving
- Covering the nose and mouth to warm the air before breathing
- Monitoring weather forecasts for wind and temperature changes
People with respiratory conditions may benefit from shorter outdoor intervals. Those with joint or muscle issues may need to stretch lightly before leaving the house to support comfort.
Hydration also matters outdoors in cold weather, as the body continues to lose moisture through breathing. Taking small precautions before stepping outside supports stability and reduces cold-related stress on the immune system.
Protecting Yourself in Public Spaces During High-Spread Months

Public spaces often increase exposure to viruses during winter. Limited ventilation, crowded indoor areas, and shared surfaces make it easier for germs to spread. People with chronic conditions benefit from simple precautions that lower the chance of infection while maintaining daily routines.
Helpful steps include:
- Washing hands after touching shared surfaces
- Carrying hand sanitizer for situations without sinks
- Avoid touching your eyes, nose, and mouth during errands
- Choosing less crowded times for shopping or appointments
- Keeping a distance from individuals who appear ill
- Wiping down carts, handles, or public equipment when possible
Face coverings may also help during high-spread months, particularly for those with respiratory or immune concerns.
Good ventilation supports safer indoor time, so individuals may choose seats near windows or doors when possible. These small precautions reduce exposure and support immune stability during winter.
Building a Simple Daily Plan That Supports Stability
Daily structure supports immune balance by creating consistent patterns that the body can follow. A simple plan reduces stress, supports nutrient intake, and helps manage chronic conditions more smoothly.
This plan does not need to be complex. A few steady habits practiced throughout the day can support balance and energy.
A supportive daily plan may include:
- A set wake time and sleep time
- A morning hydration routine
- Balanced meals spaced evenly through the day
- Light physical movement, such as stretching or short walks
- Planned breaks for rest
- A short evening routine that supports calm before sleep
- Regular symptom notes for personal tracking
This structure helps the body anticipate daily tasks and reduces unexpected physical stress. When habits stay consistent, the immune system maintains steadier patterns.
A simple plan also makes it easier to adjust quickly when symptoms change, which supports long-term stability through winter.
When to Seek Medical Guidance During Winter Symptoms

Winter symptoms sometimes require medical attention, especially for those with chronic conditions. Early guidance helps prevent complications and supports faster recovery. People benefit from knowing which symptoms signal the need for professional care.
Seek medical guidance for:
- High fever that lasts more than one to two days
- Shortness of breath or wheezing
- Persistent chest discomfort
- Sharp increases in fatigue
- Symptoms that worsen instead of improving
- Dehydration signs such as dizziness or dark urine
- Worsening asthma, COPD, heart, or metabolic symptoms
Individuals should also contact a healthcare provider if a mild illness disrupts their medication routine or causes unexpected side effects.
Winter infections often strain the body more than they do during warmer months, so timely guidance protects long-term health. Staying in communication with healthcare professionals helps maintain stability and reduces the likelihood of extended recovery periods.
The Impact of Indoor Heating on Skin and Respiratory Health
Indoor heating keeps homes warm, but it also dries the air and affects the body’s natural protective barriers. When humidity falls, moisture on the skin and inside the respiratory tract evaporates more quickly.
This can cause dryness, irritation, and increased sensitivity to germs. People with asthma, allergies, or chronic skin conditions often notice more discomfort during prolonged exposure to heated indoor air.
Common effects of indoor heating include:
- Dry or itchy skin
- Irritated throat or nasal passages
- Increased coughing
- Flare-ups of eczema or psoriasis
- Greater discomfort for individuals with asthma
Dry air reduces the mucus that normally traps germs in the nose and throat. With less moisture, the respiratory system clears irritants more slowly.
Using humidifiers, drinking more water, and opening windows for short periods can support better air quality. Regular skin moisturization and avoiding harsh soaps also help maintain comfort during winter heating periods.
Winter Health Support With My Dr’s Note
When someone becomes sick and needs documentation for work or school, My Dr’s Note offers a simple and reliable way to manage these requirements. Individuals can access a real doctor’s note through our online services. Request an online doctor’s note for work or get a doctor note online for school when symptoms affect attendance or daily responsibilities.
At My Dr’s Note, we provide a legit doctor’s note online that supports recovery without added stress. Anyone who needs to get a real doctor’s note online during winter illness can reach out for help. Every note is fully verifiable and accepted across all 50 states.
Contact My Dr’s Note today!